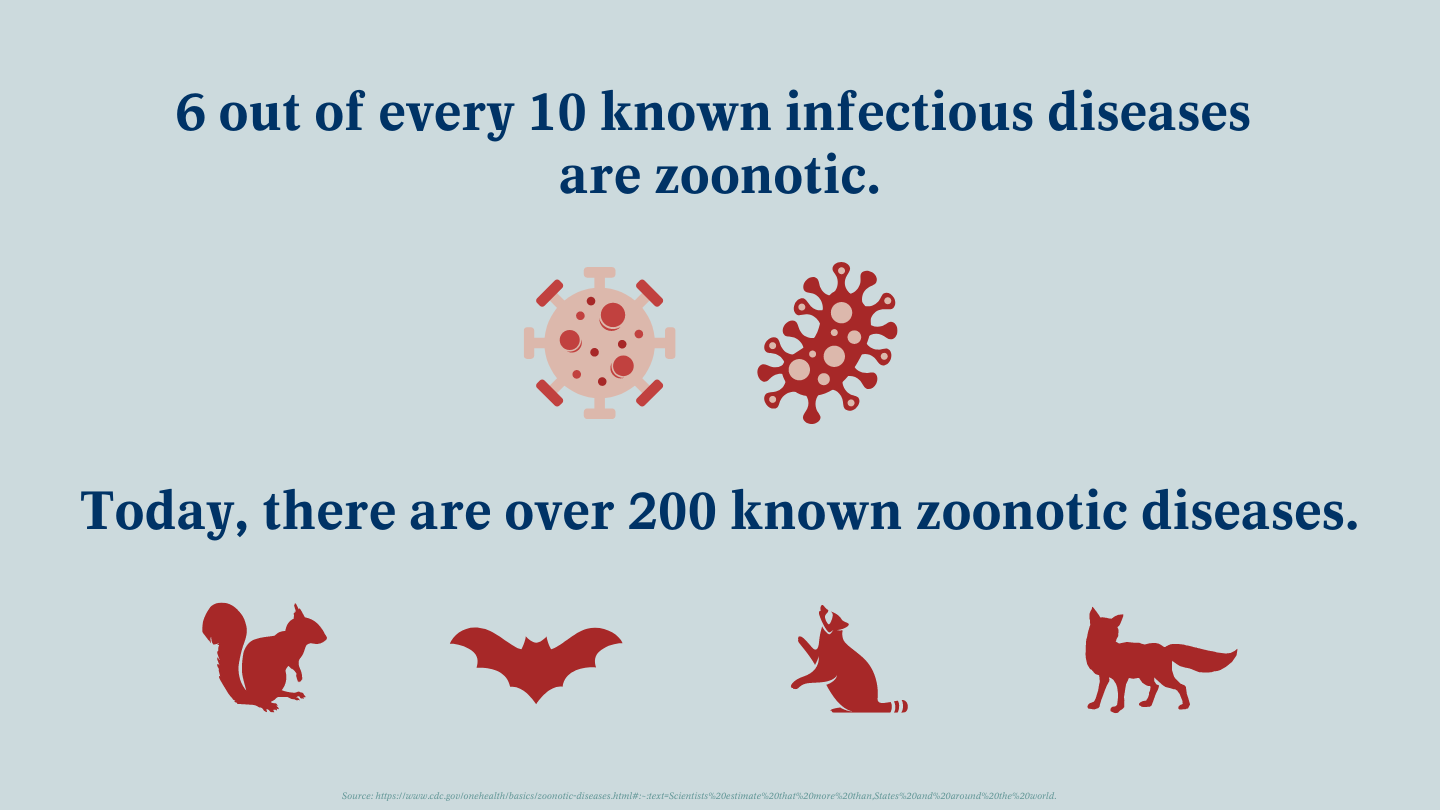
Throughout history, the intricate interplay between animals and humans has given rise to numerous health challenges. One such challenge, often overshadowed by more pressing concerns, pertains to the phenomenon of zoonotic diseases. As our understanding deepens, it becomes increasingly evident that zoonotic diseases, particularly those that arise from animal worms, necessitate closer scrutiny. This article delves into the complexities surrounding animal worms and their potential transfer to humans, offering a more nuanced perspective on an issue that is seldom fully appreciated.
Zoonotic diseases, by definition, are those that are transmissible between animals and humans. They encompass a broad spectrum of pathogens, including bacteria, viruses, and parasites. Among these, helminths, or worms, play a significant, albeit often overlooked, role. This section will explore various types of worms associated with zoonotic transmission, including roundworms, tapeworms, and flukes.
Roundworms, specifically Toxocara canis and Toxocara cati, are commonly found in dogs and cats, respectively. These nematodes can persist in the environment as eggs, remaining viable for extended periods. When humans, particularly children, inadvertently ingest these eggs—often via contaminated soil or surfaces—they risk developing a condition known as toxocariasis. This affliction, though frequently asymptomatic, can lead to serious complications if larvae migrate to internal organs such as the liver or eyes, resulting in potential visual impairment or organ damage.
Equally concerning is the threat posed by tapeworms, particularly the Echinococcus species. These cestodes are typically harbored by canines or felines and can transfer to humans through contact with contaminated feces or ingestion of contaminated food or water. Once inside the human host, Echinococcus larvae can form cysts in various organs, resulting in echinococcosis—a grave condition that can necessitate surgical intervention and, in severe cases, prove life-threatening.
Flukes, particularly those from the family Fasciolidae, represent another category of zoonotic worms that warrant attention. Commonly found in livestock such as sheep and cattle, these trematodes can infect humans when they consume contaminated water or undercooked aquatic plants. Fascioliasis, the resulting disease, can lead to acute symptoms like fever or abdominal pain, but chronic infections may result in severe damage to the liver and bile ducts, highlighting the potential for long-term health complications.
The transmission mechanisms for these worms strikingly illustrate the pathways through which zoonotic diseases can proliferate. Direct contact with infected animals or their fecal matter is a prominent risk factor, yet environmental contamination dramatically amplifies exposure. Infants and young children are particularly vulnerable due to their exploratory habits, often putting contaminated objects or soil into their mouths. Additionally, individuals engaged in agricultural or veterinary occupations face heightened risks, owing to frequent interactions with animals and their excretions.
Understanding the epidemiology of zoonotic worms necessitates a multidisciplinary approach. Environmental factors, cultural practices, and global trade play pivotal roles in disease transmission dynamics. For instance, in regions where sanitation practices are lax, the prevalence of zoonotic diseases is often significantly higher. Likewise, changes in agricultural practices and land use can disturb natural ecosystems, facilitating the spread of these helminths into new environments.
Moreover, the impact of climate change cannot be overstated. As temperatures rise, the geographic distribution of various animal-worm hosts shifts, often leading to increased human exposure in previously unaffected areas. Warmer climates can prolong the survival of viable eggs in the environment, enhancing the potential for zoonotic transmission and posing a significant public health challenge.
Preventive measures, therefore, are critical to mitigate the risks associated with zoonotic diseases. Educating the public about proper hygiene practices is paramount. Regular handwashing, particularly after handling pets or engaging in outdoor activities, can dramatically reduce the risk of transmission. Additionally, ensuring adequate sanitation in domestic and communal settings serves to diminish environmental contamination by fecal matter.
Regular veterinary care for pets, including deworming treatments, is also essential in controlling these zoonotic agents. Responsible pet ownership entails not only caring for one’s animals but also protecting the health of the community by minimizing the risk of zoonotic transmission. Furthermore, food safety practices, such as proper cooking of meat and thorough washing of fruits and vegetables, significantly lower the likelihood of infection.
Public health initiatives targeting at-risk populations—such as farmers, veterinarians, and childcare providers—should be prioritized. Creating awareness campaigns, providing resources for education, and facilitating access to healthcare can enhance early detection and management of zoonotic diseases. Policymakers ought to consider reinforcing regulations surrounding animal husbandry and waste disposal, further curtailing the spread of infectious agents.
In conclusion, the interplay between animal worms and human health underscores the intricate tapestry of zoonotic diseases. While the transmission of helminths poses tangible risks, enhancing awareness and implementing preventive strategies can significantly mitigate these hazards. As we traverse the complex nexus of animal and human health, a proactive and informed approach is vital in safeguarding public health and fortifying our defenses against these insidious zoonotic threats.