When it comes to gastrointestinal health, the necessity of robust bowel preparation cannot be overstated. The Boston Bowel Preparation Scale (BBPS) is a pivotal tool employed by medical professionals to gauge the effectiveness of bowel cleansing prior to procedures such as colonoscopy. This scale not only serves to enhance the quality of these procedures but also significantly impacts patient outcomes. Understanding what the BBPS measures and the importance of these measurements can empower patients and caregivers alike, leading to better overall health management.
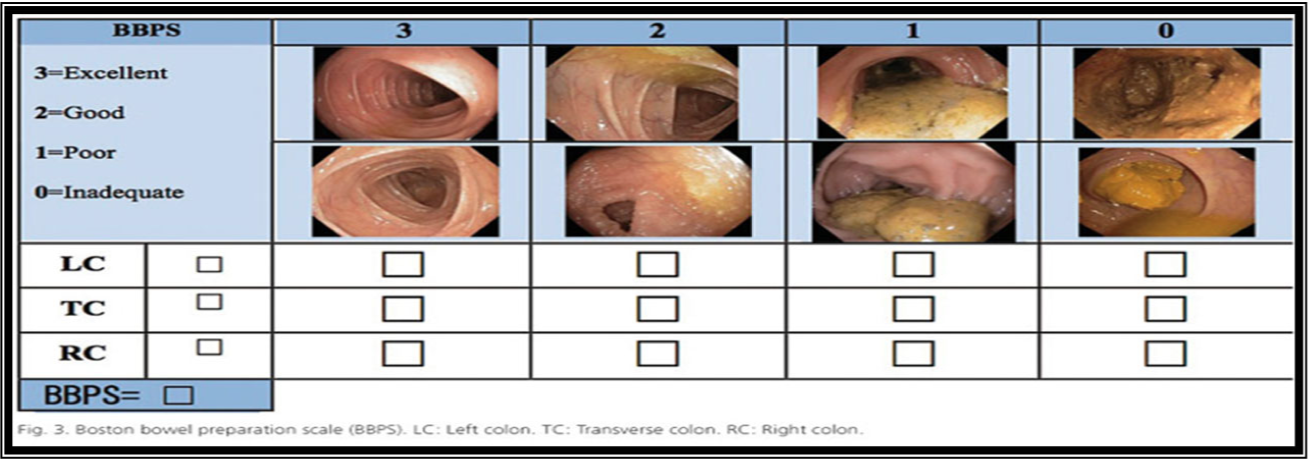
Originally developed as an objective measurement tool, the BBPS assesses the cleanliness of the colon, categorizing findings into distinct sections. It comprises a three-point scale that evaluates the right side, left side, and rectum of the colon. Each aspect is assessed independently and receives a score ranging from 0 to 3, with 0 indicating no preparation and 3 representing an excellent level of cleanliness. Collectively, scores can range from 0 to 9, guiding healthcare providers in determining whether a patient has adequately prepared for their colonoscopy.
The BBPS elucidates the three major regions of the colon: the ascending colon on the right side, the transverse colon at the top, and the descending colon to the left. Additionally, the rectum is assessed independently. This division allows for a nuanced understanding of bowel cleanliness, enabling clinicians to pinpoint specific areas that may not have been adequately prepared. The need for thorough cleaning is accentuated by the fact that residual fecal matter can obstruct the visualization of significant pathologies, including polyps or tumors, which in their precancerous state pose a great risk to patient health.
The implications of a good bowel preparation score extend beyond immediate procedural efficacy. A well-prepared bowel can lead to reduced procedural times, lower rates of complications, and less discomfort for the patient during and after the colonoscopy. Conversely, poor preparation can result in repeat procedures, which can be both inconvenient and distressing for patients, not to mention the additional healthcare costs incurred. This scalability of preparation effectiveness serves to underscore the scale’s overarching significance in clinical practice.
In a contemporary healthcare landscape that prioritizes patient-centered care, deploying the BBPS acts as a cardinal measurement for providers. It ensures that patient interactions focus not only on the technical feasibility of a procedure but also on the quality of the experience itself. Furthermore, the BBPS has been validated through extensive research and multi-center studies, further solidifying its role as a gold standard in bowel preparation assessment.
The clinical relevance of the BBPS cannot be overlooked. Studies have demonstrated a direct correlation between high BBPS scores and favorable clinical outcomes. For example, patients whose bowel preparations were rated ≥6 are significantly less likely to require repeat colonoscopies compared to those with lower scores. The metric encompasses a wealth of underlying factors, all hinting at the direct relationship between preparation quality and detection rates of colorectal anomalies.
Moreover, it is essential to note the procedural implications against the wider backdrop of colorectal cancer, which remains one of the leading causes of cancer-related mortality. Early detection is critical, and a clean visual field during colonoscopy allows for more reliable assessments. Therefore, the BBPS becomes a fundamental part of the colorectal cancer screening narrative. As such, education about bowel preparation—beginning with clear communication regarding dietary restrictions, hydration, and timing—can significantly improve BBPS scores among patients.
Beyond its clinical utility, the scale serves as a touchstone for patient engagement. Ensuring that patients are adequately informed about the importance of bowel preparation may mitigate anxiety surrounding the procedure itself. Clear instructions coupled with supportive counseling can enhance compliance and ultimately lead to improved BBPS scores. Furthermore, clinicians can adapt their approaches based on the BBPS findings, tailoring follow-up interventions for those who may struggle with bowel preparation.
The role of healthcare providers in this process cannot be understated. It is incumbent upon them to foster a collaborative environment where patients feel comfortable discussing their concerns. Research indicates that patients who engage actively in their healthcare decisions generally exhibit greater adherence to preparatory protocols. Therefore, the BBPS can be utilized as a conversation starter, laying the groundwork for candid discussions between healthcare providers and patients regarding preparation methods.
In conclusion, the Boston Bowel Preparation Scale is not merely a metric; it is a comprehensive tool that encapsulates the crux of effective bowel preparation for colonoscopy. By evaluating cleanliness in a systematic manner, it has validated the premise that thorough preparation is indispensable for optimizing patient outcomes. Healthcare professionals and patients alike must be cognizant of its valuable implications, reinforcing the essence of attentive preparation and proactive health management. As the medical community continues to advocate for enhanced screening practices, the BBPS stands out as a beacon of excellence in gastrointestinal healthcare.
Understanding the significance of the BBPS can profoundly affect patients’ experiences and outcomes, making it a critical element of modern healthcare practice. Awareness and diligence in the preparatory phase can contribute to more effective procedures, better health outcomes, and ultimately, a more profound understanding of individual well-being.