In the realm of medical science, the concept of blood transfusion has become a fundamental intervention to save lives and treat diverse conditions. Traditionally, human blood has been the gold standard for transfusions, owing to its unique composition and compatibility factors. However, the notion of utilizing animal blood in humans has invoked both curiosity and controversy. Can animal blood truly be transfused to humans? As we delve into the intricate science behind cross-species transfusions, we will explore the potential, challenges, and implications of integrating animal blood into human medicine. This discussion is underscored by the necessity for deep understanding and ethical considerations regarding blood compatibility.
To grasp the complexities of using animal blood, we must first understand blood composition in both humans and animals. Blood serves as a vital fluid, carrying oxygen, nutrients, hormones, and waste products throughout the body. In humans, blood comprises red blood cells, white blood cells, platelets, and plasma, each playing instrumental roles in maintaining homeostasis and immune responses. Similarly, animal blood exhibits analogous components, though the specificities can differ drastically across species.
One of the foremost scientific concerns in transfusing animal blood to humans is the principle of immunological compatibility. The immune system is a highly discerning entity orchestrated to identify foreign bodies. When non-human blood is introduced into a human recipient, the likelihood of an adverse immunological response is exacerbated due to the presence of different antigens. Antigens are proteins found on the surface of red blood cells that stimulate immune reactions. Notably, many animal species possess unique antigens that can provoke a robust immune response, leading to complications such as hemolytic reactions, where the body inadvertently destroys the transfused blood cells.
Despite these challenges, researchers have explored specific instances where cross-species transfusions may be beneficial. For instance, certain large mammals, like pigs, contain blood that has comparative physiological properties to humans. Porcine blood, for example, has garnered attention due to its high levels of hemoglobin, which could theoretically enhance oxygen transport in critical medical situations. Trials have been conducted to ascertain the viability of utilizing this animal blood in dire circumstances when human blood supplies are exceedingly limited. Nevertheless, the results remain inconclusive, and more extensive clinical studies are warranted to elucidate potential risks and benefits.
Beyond physiological compatibility, ethical considerations loom large in the discourse surrounding animal blood transfusions. The sourcing of animal blood raises questions regarding animal welfare and the sustainability of such practices. Harvesting blood from animals for medical use could entail invasive procedures, inciting debates regarding humane treatment. Furthermore, potential zoonotic transmission of diseases—pathogens that can jump from animals to humans—poses a significant threat. These pathogens—including various viruses and bacteria—could significantly compromise public health if animal-derived blood were adopted in human transfusion protocols.
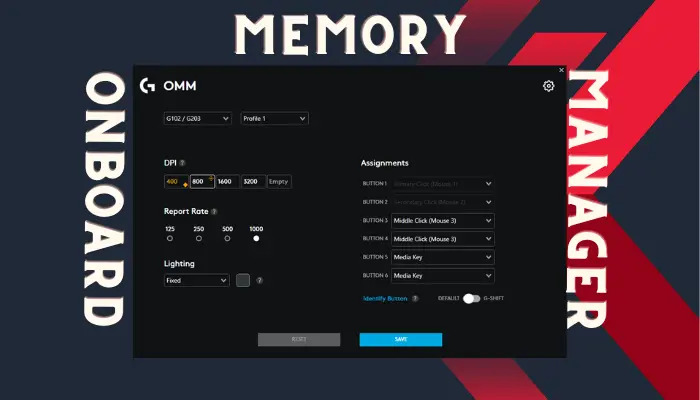
There is also the looming challenge of regulatory frameworks governing blood transfusions. Blood banks and healthcare institutions are governed by stringent standards to ensure safety and efficacy, primarily focused on human blood. The introduction of animal blood transfusions would necessitate a comprehensive re-evaluation of these criteria to evaluate not only the biological compatibility but also the ethical sourcing and potential public health implications. This rigorous regulatory landscape can be a daunting hurdle for proponents of integrating animal blood into therapeutic avenues.
Interestingly, researchers have posited alternative strategies to mitigate the risks associated with animal blood transfusions. Innovations in biotechnology have led to the exploration of creating synthetic blood products—hemoglobin-based oxygen carriers—that could replicate the properties of real blood without the complications arising from cross-species transfusion. Such advancements could circumvent the issues associated with immunological rejection and zoonotic diseases, providing a potentially safer option for those in need of transfusions.
In recent years, xenotransfusion—the practice of using animal blood or organs for human use—has been a focal point for scientific inquiry. The success of xenotransplantation (transplanting organs from one species to another) has sparked interest in whether the same principles can apply to blood transfusions. While research continues to evolve, successful applications remain sparingly documented, and the intricacies of this field demand cautious optimism rather than exuberant enthusiasm.
As we reflect upon the multifaceted dimensions of cross-species transfusions, the consensus remains that the prospect of using animal blood in human medicine is laden with complex challenges. While the potential may exist under specific circumstances, any attempts to integrate such practices must be approached with meticulous precision, acknowledging the risk factors and ethical implications at play.
Ultimately, as science advances, the aspiration to uncover novel solutions for blood shortages may pave the way for unconventional avenues. However, it is imperative to maintain a careful balance between innovation and ethical responsibility. While the promise of healing drives research forward, the health and well-being of both human and animal subjects must remain paramount. In the world of medicine, the intricacies of blood transfusion illustrate one of the many pressing dilemmas where science, ethics, and humanity converge, revealing the complex tapestry of life and its inherent connectivity.